America’s Health Care System is Even More Broken than You Think
America’s Health Care System is Even More Broken than You Think
How did private insurance companies come to control U.S. health care—and make our coverage the most expensive in the world?
Congressional Republicans are closer to fulfilling their party’s long-held promise to revoke the Affordable Care Act. Now that the House has passed a repeal bill, Senate Republicans are busy hammering out their own version behind closed doors.
Yet, for advocates of universal health care, things might not be quite as grim as they seem.
In order to gain votes from both conservatives and moderates in their party, Republican leaders leaders beat, tortured, and dragged their bill through the House. They ended up with a battered legislative heap containing just enough jagged boards and exposed nails to injure voting groups all along the ideological lane. The backlash has been swift and fierce. After passing the bill, House Republicans returned to their districts to find contentious town halls and angry voters. “Mean-spirited,” “a betrayal,” and “cruel” are but a few of the words used to describe how the bill unravels ACA Medicaid expansions and underfunds—thereby jeopardizing—coverage for people with preexisting conditions. Meanwhile, conservative and right-leaning think tanks have panned the bill for leaving the ACA’s basic framework in place. Even Trump supporters on talk radio must continually assure audiences that the bill is only a first step toward the conservative vision of health care. The bill inspires no one or, at least, no one I have yet encountered. Nor does there seem to be much enthusiasm about what Senate Republicans might produce.
So why the optimism?
First, reaction to the House bill demonstrates the difficulty of rolling back guaranteed care once it’s in place. Most voters, including substantial numbers on the right, have come to expect a government solution to health care and very few want to see a system that leaves the working poor or chronically ill without insurance.
Second, both Republicans and Democrats are in an uncomfortable political position. The Republicans are staring down the barrel of a gun called public opinion. If their bill manages to eke through the Senate and become law, then the GOP will be on the hook for every failure in U.S. health care, from vulnerable populations left uncovered to rising premium prices. For their part, Democrats recognize that the ACA has significant flaws and requires further reform. Premium prices on the state exchanges are rising annually at a clip of 10, 20, even upwards of 30 percent while some beneficiaries have deductibles so large that their coverage, unless they get cancer or are hit by bus, is nonexistent. Rising costs have encouraged insurance companies to pull out of exchanges, leaving some regions without an ACA provider. If the Republicans fail to pass their bill, Democrats will be saddled with the legacy of failing to live up to the promises of universal health care. This bipartisan political bind may just be enough to compel both parties to work together on fixing the ACA.
At bottom, though, is a deeper challenge. American health care is a monstrosity, a tangle of private and governmental power that is both expensive and inefficient. Thanks in large part to the advocacy of Bernie Sanders, “Medicare for All” has become a rallying cry on the left. However, universalizing Medicare would leave insurance companies at the center of the health care system and would fail to address underlying problems that make U.S. coverage the most expensive in the world. Only fundamental reforms that reduce corporate influence over health care can make generous universal coverage possible.
It has taken a long time to create today’s profoundly broken system. To understand how we got here and where we should go next, a little history is required.
For the better part of a century, U.S. health care has been structured around a particular corporate model that was concocted—practically out of thin air—by the American Medical Association (AMA). During the Great Depression, AMA leaders created what I call the “insurance company model” to defeat numerous, existing health care arrangements that they believed did not go far enough in protecting physician autonomy and pay. The AMA got its way, but the venture did not turn out as its leaders had expected.
The critical thing to understand about the insurance company model is that it developed so that insurance companies no longer simply finance medical services—now they also influence the way medicine is practiced. Over several decades, the insurance company model evolved to weaken the position of doctors while endowing corporations with enormous power over health care. Today’s insurers oversee physician work, both in their capacity as private-sector financiers and as they help administer government programs like Medicare. Insurers decide which drugs and procedures receive coverage and compel physicians to follow treatment blueprints in exchange for reimbursement. If insurance companies refuse to cover a medical procedure, it might as well not exist.
This outcome would have been impossible to imagine not so long ago. During the first half of the twentieth century, the health care market supported myriad financing and delivery arrangements. Labor unions, farmers’ associations, consumer cooperatives, and mutual aid societies supplied medical services to members without any insurance company involvement. Unions, for example, contracted directly with physicians and hospitals to create their own health care networks. Many of these plans were skillfully managed to hold down expenses. They frequently paid doctors set salaries or per-patient fees, used point-of-service deductibles, and provided free preventative care to reduce long-term costs.
One popular model, admired by progressive reformers and patients alike, was the prepaid physician group. (Today, similar though not exact replicas of these groups are being revived under the label of “cooperatives” or “community health care plans.”) These prepaid doctor groups staffed general practitioners and doctors from a variety of fields, including surgery, obstetrics, and optometry. Unlike in today’s fragmented system, patients could access comprehensive health care in one place while doctors from across specialties routinely met to discuss how to holistically manage complex cases.
Patients who belonged to these plans paid a set monthly fee in return for care from both the physician group and the hospital with which the group contracted. Group doctors owned the risks associated with treating patients, which tied their compensation directly to the bottom line. This financing structure forced doctors to balance the dueling goals of providing excellent care while avoiding “overutilization,” or an oversupply of services. If group physicians delivered unnecessary services, they took money out of their own pockets. But if doctors, hoping to save a buck, withheld necessary patient care, then they would lose revenue in the long run. Patients would become sicker and costlier for want of preventative or necessary services while the group would lose customers unwilling to pay for inferior care.
Despite the success of such medical programs, the AMA launched a full-scale assault against these so-called “alternative” forms of care. The leaders of organized medicine feared that the plans could develop into corporations that would bureaucratize medicine, thereby reducing physicians’ autonomy and pay. AMA officials used their influence to revoke the medical licenses and hospital admitting privileges of noncompliant doctors, which shuttered many plans and stopped the expansion of any that managed to survive.
The AMA’s recalcitrance handed reformers an invitation to seek government intervention in medicine. The invitation was taken up during the Great Depression by New Dealers who initiated what would become a decades-long campaign for federally funded health care benefits.
Under this political pressure, AMA leaders invented the insurance company model. After decades of stymieing the health care sector, association officials concluded that they needed a program they could pitch as an alternative to government intervention. AMA leaders decided that insurance companies—not labor unions, physician groups, consumer cooperative, or mutual aid societies—were their best hope.
Doctors gambled that they could restrain corporate power by requiring insurers to grant them autonomy to practice medicine as they saw fit. Because insurance companies were geographically removed from most physicians—generally headquartered in a distant city from the doctor whose services they funded—AMA officials believed their members could escape corporate oversight. Fear of bureaucratized medicine also led the AMA to oppose multispecialty physician groups, which they viewed as nascent corporations. This decision eviscerated holistic care. No one doctor or doctor group would have responsibility for the patient’s overall health. Instead, patients would have to coordinate their own medical program as they were shuffled from one specialist to another. Crucially, the AMA also demanded that insurance companies pay doctors for each and every service provided. Fee-for-service payment, in lieu of set salaries or per-patient fees, incentivized doctors to oversupply services to the insured.
Almost everyone—from insurers to health care experts to politicians—recognized that the insurance company model encouraged physicians to oversupply services, pad bills, and then send off the invoice to an insurance company located far away. Even insurers were reluctant to participate in the AMA’s plan, but they eventually gave in because they wanted to defeat nationalized medicine.
Because it produced an expensive product, the insurance company model got off to a lackluster start. By 1945, only about one-quarter of the population owned insurance and benefits were stingy, usually covering only a portion of hospital costs.
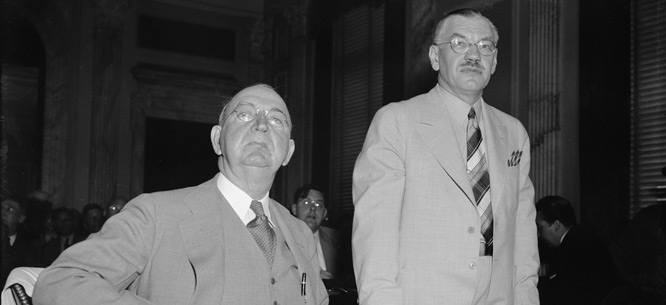
Against this backdrop, Harry Truman launched his bid for universal health care. Recognizing the inefficiency of the insurance company model, administration officials planned to reduce costs by restructuring the health care system and resuscitating prepaid physician groups. The AMA joined with insurers and other business interests to defeat universal care. But they did not emerge from the debates unscathed. Both Democrats and Republicans demanded that private interests prove they could expand coverage and provide more benefits. For politicians bent on establishing the superiority of the U.S. system over the Soviet system, it was important to showcase a health care sector that covered the vast majority of citizens and provided generous benefits. Even conservative and moderate legislators who had opposed Truman’s bill offered their own reform proposals, albeit with more modest plans for government intervention.
To defeat reformers, physicians and insurers had to demonstrate the strength of the insurance company model. Whether in private meetings or in congressional testimony, physicians and insurers depicted expanding and improving coverage as the essential weapon in their battle against federalized health care. Not that they were entirely averse to government support. Under Eisenhower, policymakers formalized tax reductions for employers who supplied fringe benefits to workers. In this way, the government subsidized business purchases of insurance company products, further boosting private-sector coverage numbers.
Private attempts to prove the insurance company model’s virtue produced dramatic results. Between 1945 and 1965, the percentage of Americans with some form of medical insurance increased from approximately 25 percent of the population to almost 80 percent. Benefits also became far more generous, expanding beyond hospital care to also include physician office visits, preventative medicine, and diagnostic services.
As insurance coverage expanded, health care costs ballooned. Since the end of the 1940s, escalating medical costs have outstripped increases in every other category measured by the Consumer Price Index. With rising costs undermining claims about the insurance company model’s strength, physicians begrudgingly accepted insurers’ procedures to limit costs.
Through cost controls, insurance companies gradually moved beyond financing medical services to also managing medicine. Beginning in the 1950s, insurance companies established utilization review committees to monitor physician services and identify where unnecessary tests or procedures ran up the insurance bill. Physicians responded by tailoring their practice to accommodate insurance billing procedures. By the 1970s, doctors who failed to comply with insurers’ standards for medical care either received a warning or were denied reimbursement altogether.
Despite the extraordinary growth of private insurance, high policy costs prevented insurance companies from extending protection to a politically satisfactory percentage of the elderly. To address this problem, politicians established Medicare in 1965.
Unfortunately, Medicare retained the insurance company model. Longtime reform advocates and policymakers in the Social Security Administration were loath to design the biggest breakthrough in federal health care programming around the private market’s defective, high-cost structure. They realized, however, that after decades of development, the insurance company model had amassed significant organizational capacity and cultural authority. The private sector had matured ahead of the public sector. By the 1960s, insurance companies seemed better equipped to manage a large health care program than did a public agency attempting to reinvent the wheel.
Americans had grown accustomed to the insurance company model. Consumers and physicians had adapted to insurance company policies. So had union leaders, who now focused their energies on improving their employer-provided benefits. By adopting insurance company arrangements, Medicare’s planners could surmount administrative obstacles and present their program as a replica of the health care arrangements with which patients and providers were already familiar.
Enhancing Medicare’s corporate flavor, policymakers granted insurance companies an administrative role by designating them as intermediaries between the government and health care providers. Insurance companies process Medicare claims and payments, investigate reimbursement and fraud issues, enroll health care providers, manage provider questions and communications, and educate hospitals and physicians about billing procedures or changes.
By working within the insurance company model, Medicare inherited the private sector’s shortcomings. Physicians continued, as they usually are today, to be paid for every service they provided, thereby encouraging them to over-deliver care to the insured. Government support increased the demand for health services, but the insurance company model could not handle this demand and costs skyrocketed. Meanwhile, efforts to constrain the service supply and control costs have led to standardized medical regimens that undermine patient treatment options and prevent doctors from creatively and innovatively practicing medicine.
Some progressive policymakers hoped the Affordable Care Act would displace the insurance company model. They called for a public option that would supply consumers with a government-managed insurance policy. By loading up these policies with generous benefits and pricing them at costs below what insurance companies could offer, reformers planned to gradually weaken private-sector insurance. However, the public option failed to garner sufficient congressional support. In the final legislation, reformers managed to include provisions for Accountable Care Organizations and nonprofit health cooperatives, once again attempting to supplant insurance company dominance. However, federal directives and reporting burdens made it difficult for physicians and community groups to break free from the status quo and launch their own health care plans. Thus, Americans were left with another federal program that, like Medicare, was trapped within the confines of the insurance company model.
Taking a page from history, progressive policymakers should work to fundamentally restructure health care so that plans resembling earlier community programs run by doctor groups, unions, and consumer cooperatives can flourish. A universal system that grants individuals subsidies to purchase coverage from any medical plan—not just insurance companies—would effect this change.
It’s a simple plan for universal care. But it’s also a plan that will drastically reduce costs, encourage doctors to find innovative health care solutions, and liberate the system from corporate control.
Christy Ford Chapin is an associate professor in the University of Maryland Baltimore County’s history department and a visiting scholar at Johns Hopkins University.