Unhealthy Boundaries
Unhealthy Boundaries
A neoliberal vision of public health and anti-immigrant politics have turned healthcare into a border zone.
When we think about the hostile environments governments have created for migrants in recent years, we often picture militarized borders, detention centers, and police empowered to harass and deport. Amid these powerful images of maltreatment, it’s easy to miss less sensational forms of violence that migrants face under foreign governments. One of the most harmful is the way healthcare is used to deny migrants the conditions of life itself.
In Greece on July 17, newly appointed Labor Minister Yiannis Vroutsis revoked a law passed only a month earlier by the Syriza-led government that granted National Health Care services to all foreigners from non-EU countries, including refugees, without exceptions. “Our country is not an unfenced vineyard,” Vroutsis tweeted while announcing the decision. The 2010 Affordable Care Act in the United States extended coverage to the uninsured but excluded undocumented immigrants. At detention centers near the Mexican border, migrants lack access to basic healthcare, alongside amenities like nutritious food, soap, and toothpaste.
The new NHS Visitor and Migrant Cost Recovery Programme in the UK restricts free access to hospital care for migrants who are deemed to be in the UK in order to access its health and welfare system. The British Medical Association describes the regulations as contravening the ethical obligations of the medical profession and condemns them as fundamentally racist. The government has also put in place a statutory requirement for NHS Trusts to charge migrants up to 150 percent of costs upfront for most types of medical care, withholding treatment if a patient can’t pay. Doctors are placed in the perverse position of “managing” without treating the conditions of patients who can’t pay for care. And migrants aren’t just denied healthcare provision; they are punished for seeking it out. Victims of trafficking and sexual exploitation are being arrested after seeking emergency care. Bailiffs are being sent by NHS trusts to take debts from destitute individuals.
In Turkey, where I currently live, undocumented migrants are not entitled to access public healthcare. While they technically have access to free emergency services, some choose not to go to hospitals out of fear of being arrested (in November 2018 the Ministry of Health held a meeting with the directory of public hospitals in Istanbul stating that undocumented migrants should be reported to the police immediately upon entrance to public hospitals). Their only option is to seek private care, where they can be charged higher prices under medical tourism regulations.
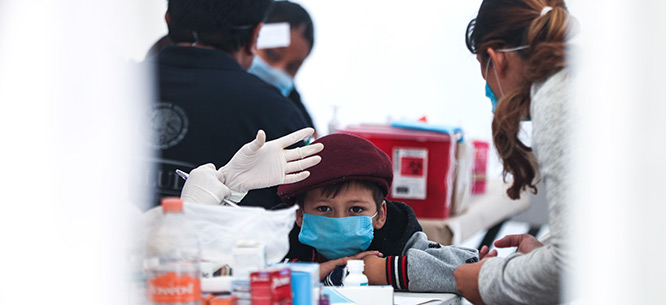
Thousands of these migrants in Turkey are Afghans, Iranians, Somalis, and Iraqis, many of whom faced harassment, persecution, or torture in their country of origin, often for their sexual orientation. Registered asylum seekers, including Syrian refugees under Temporary Protection Status, are technically entitled to free care in the cities in which they’re registered but face myriad barriers in accessing services. As a result, women are forced to give birth at home, babies are dying, and marginalized members of the population are not receiving essential vaccinations.
These policies are justified on grounds that migrants should “Make a Fair Contribution” (from the title of a UK White Paper) to services that are paid for by taxpayers’ money or through private insurance. Many of these countries have health systems operating under conditions of austerity or privatization; in many cases, it isn’t only migrants but citizens priced out of services whose right to healthcare is denied. Both groups are embedded in the same political-economic system that led many migrants to leave their homes in the first place. Neoliberal public health regimes and anti-immigrant politics have turned healthcare into a border zone.
Exhausted and Expendable in Turkey
An Afghan man falls sick while working in a workshop in Zeytinburnu district of Istanbul and becomes paralyzed. His boss doesn’t help him, but his friends take him to a pharmacy. From there they refer him to a hospital, but the hospital refuses to see him without an identity card. His friends buy a ticket to fly him to Afghanistan and take him to the airport, but he’s too sick to travel. At the airport he’s picked up by the police, who take him to the hospital where he’s treated for forty days. He dies there. His friends go to the Afghan Consulate to request help in sending his body back to his family, but the consulate doesn’t help. The people from his village raise $1,300 in order to bring his body back.
An eighteen-year-old Afghan man is working in a plastic factory in the Bayrampaşa district in Istanbul and becomes injured when a piece of plastic flies into his eye. He loses his vision and is fired from his job as a result. He waits for two weeks and then goes to a private hospital for treatment, but can’t afford the cost (7,000 TL, or about $1,200), so he is forced to go back to Afghanistan.
A Senegalese woman is arrested by the police for not having documents when the authorities come to remove her husband’s dead body.
An Afghan man is shot in the leg and is imprisoned rather than receiving treatment.
In Turkey, undocumented migrants and asylum seekers who fall out of the system of care face insecurities related to their means of making a living, their housing conditions, and their vulnerability to deportation. Undocumented women are targeted for sexual abuse specifically because they are too afraid to access emergency health treatment.
Most undocumented migrants work in Turkey in labor-intensive informal spaces with poor health and safety regulations. Men work in textile, leather, or metal workshops; construction; waste-paper collection; street selling; or a variety of forms of casual day labor. Women find work in textile and garment workshops, as well as domestic care work, entertainment sectors, and the sex industry. The rate of workplace accidents is very high (2,006 workers were killed in workplace accidents in 2017 in Turkey), and the payment very low—200 TL (about $35) per week according to a preliminary observation report made by Ankara Occupational Health and Safety Council.
Many of the areas in which migrants live in Istanbul are characterized by poor housing that the government has marked for future renovation but is falling into disrepair, or that has been neglected entirely. Poor ventilation, heating, sanitation, and cooking facilities all bear on their occupants’ health. Young migrants may share a bed, taking it in turns to sleep, and pay their rent by the hour. These conditions don’t just affect physical health; taken in combination with frequent threat of arrest and deportation, exploitation in the workplace, and the loneliness that comes with such a fragmented lifestyle, migrants also face severe challenges to their mental and emotional well-being.
Migrants still find ways to circumvent legal barriers to healthcare. They borrow identity cards from documented friends, use inside contacts, receive treatment from unregulated backstreet providers, or borrow money. But these survival tactics are stopgaps, which only create more opportunities for exclusion and exploitation.
Multiple Borders
Borders are not only lines on a map or concrete walls impeding physical movement. They come into being through many interactions and transactions. They mark who is excluded and included in a variety of institutions and ways of life. Employers in insecure work spaces, landlords of cheap housing, police on the street, lawmakers, the bureaucrats who administer laws, friends and family members, and the health workers—doctors, hospital receptionists, pharmacists—all play a role in determining who belongs and who doesn’t. And the more unequal a society is, the more those at the bottom, whether citizen or migrant, lack the rights that those at the top take for granted.
In other words, migrants, despite facing the most acute exclusions, aren’t the only ones being kept out. A well-known Alevi folk singer, Ali Nurşani, recently made a public video requesting financial support to assist in paying for his son’s cancer treatment. A retired worker with social security, he was unable to access the treatment in public hospitals because they were over capacity and have inefficient appointment systems, and he couldn’t afford the cost of care in private hospitals. The healthcare border enters into the lives of precarious Turkish citizens alongside those migrants fully excluded from the system.
The logic of austerity harms migrants and non-migrants alike. Rather than doubling down on policies that exclude non-citizens, more investment in public health could benefit all who need care—a political project where the needs of migrants are recognized alongside the needs of citizens, because so many of their problems stem from common causes.
Helen Mackreath is the Middle East Correspondent for the Los Angeles Review of Books. She is currently researching issues relating to Syrian refugee governance in Turkey.
Fattah Lemar Rabiei contributed to this piece.