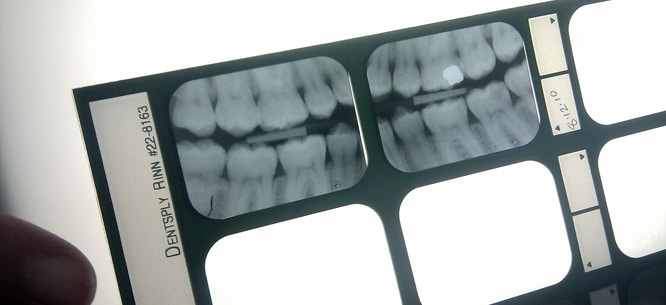
The Class Politics of Teeth
The Class Politics of Teeth
Inequalities in oral health and dental access reflect our deepest social and economic divides.
On a cold fall morning, about four hundred people lined up on the outskirts of the mountain community of Jonesville, Virginia. News had spread about a free weekend health clinic, organized by the Knoxville, Tennessee–based Remote Area Medical Volunteer Corps, or RAM.
Since it was founded more than three decades ago, the nonprofit has headed hundreds of missions, airlifting medical relief to some of the poorest places on the planet. This was RAM’s first visit to this isolated pocket of Appalachia, in 2014. The clinic was offering a wide range of services, everything from chest x-rays to eye exams. An overwhelming number of people in the line, however, were worried about their teeth.
“I’ve got a couple of broken ones and a couple of bad cavities,” Randy Peters, a fifty-one-year-old former miner and mattress factory worker with multiple sclerosis, told me. “It’s getting so I can’t eat.”
Ernest Holdway, a disabled miner in his early sixties, said he came to get a tooth extracted. “It ain’t hurting but it will,” he predicted. He said his dental insurance ended when he left the coal mine. He said he just finished paying off the $1,500 he owed for the extraction of three bad molars, which he was told to get removed before a knee surgery. He was still fighting to save his leg, which looked fearfully swollen.
“I’m a good person but I sure have been tested,” he added.
In poor and remote Lee County, where Jonesville is located, shortages of all kinds of healthcare have been a chronic problem, but the dearth of dental care has been most acute. Lee County is not alone. By federal estimates more than 50 million Americans live in communities that face a federally designated shortage of dental professionals. Their teeth suffer and so does their general health. Pain is common. During free clinics like these, hundreds, sometimes thousands of ruined teeth are extracted.
Scenes such as these, which I observed over the decade I spent writing a book on America’s dental care system, illustrate the obstacles many Americans face in obtaining proper dental care. Due to economic deprivation, geographic isolation, age, disability, and lack of dental coverage, an estimated one-third of the population faces significant difficulties getting access to the autonomous, insular, and privatized system that provides most of the dental care in this country. Dentists are healthcare providers, yet are also small business people. They thus tend to set up private practices in affluent metropolitan areas that they hope will offer a good return on their investments in education, equipment, and staffing. As a result, they are in short supply in many poor, minority, and rural communities, as are dental benefits and money to pay for care.
Meanwhile, the healthcare safety net—incomplete as it is for medical care—has even greater deficiencies when it comes to oral health. There is no universal dental coverage, of course. But additionally, even Medicaid, which provides healthcare coverage to about 74 million poor Americans, treats adult dental benefits as optional. Although children are entitled to dental care under Medicaid, fewer than half of children covered by the program obtain dental services, while fewer than half of the nation’s dentists participate in the program, citing low reimbursement. And Medicare, which provides healthcare coverage to roughly 55 million elderly and disabled Americans, has never included routine dental benefits, leaving millions of beneficiaries uninsured.
So people line up at these free clinics desperate for dental services. “These are not forgotten people,” RAM dental director John Osborn, a Knoxville dentist, explained in Jonesville. “The system has passed them up.”
Inequalities in oral health and dental access reflect our deepest social and economic divides. The “Hollywood Smile” has become a status symbol around the world, and better-off Americans routinely pay for elective procedures ranging from teeth whitening and veneers to complete “smile makeovers” costing many thousands of dollars. Meanwhile, more than one out of three low-income American adults avoids smiling because of poor oral health, according to a poll conducted for the American Dental Association (ADA) in 2015.
Ashamed and stigmatized, the poor are shut out of opportunities for social advancement as well as work that could help them escape poverty. “If you have lousy teeth, you can’t get a job,” observed Philip Alston, United Nations Special Rapporteur on extreme poverty and human rights. Alston was speaking in Washington, D.C. in December 2017 at the conclusion of a fact-finding mission to study extreme poverty in the United States, one of the world’s wealthiest countries.
In visits to homeless encampments in California, storm-devastated areas of Puerto Rico, and poor communities in Appalachia and the Deep South, Alston said he observed evidence of many serious health conditions. But he expressed a special concern for the dental problems of America’s poor.
The shortage of oral health services combined with the pain and stigmatization of oral disease “fundamentally affect the human dignity and ultimately the civil rights of the persons concerned,” Alston noted in a statement he issued at the end his trip. International human rights law recognizes the rights to an adequate standard of living and to healthcare as basic human rights, he observed. The United States, which has not ratified the International Covenant on Economic, Social and Cultural rights, does not.
“In practice, the United States is alone among developed countries in insisting that while human rights are of fundamental importance, they do not include rights that guard against dying of hunger, dying from lack of access to affordable healthcare, or growing up in a context of total deprivation,” Alston stated.
In his investigation, Alston aimed to determine whether conditions that burden and shorten the lives of the poor actually breach the rights they are granted under the U.S. Bill of Rights or the International Covenant on Civil and Political Rights, to which the United States is a party. His final report will be presented to the UN Human Rights Council in Geneva in June.
The struggle over the recognition of healthcare as a human right has been a long one in the United States. Yet often, when dental services have been mentioned at all, they have remained a marginal part of the debate. But this may be changing.
In 2000, then U.S. Surgeon General David Satcher reframed dental disease as oral disease and oral disease as a public health crisis. In his landmark Oral Health in America report that year, Satcher warned that from cavities to gum disease to oral cancers, a “silent epidemic” was raging in our nation.
“Those who suffer the worst oral health are found among the poor of all ages, with poor children and poor older Americans particularly vulnerable,” Satcher noted in his report, the U.S. government’s first-ever comprehensive study of the nation’s oral health. “Members of racial and ethnic minority groups also experience a disproportionate level of oral health problems,” he noted. “Oral health means much more than healthy teeth,” stressed Satcher, a physician by training. He urged recognition of the fact that “oral health and general health are inseparable.”
Oral Health in America ended with a call to action: an appeal for increased research, removing barriers to care, raising awareness about oral health among citizens, lawmakers, and healthcare providers, rethinking how the oral health workforce operates, and building an American healthcare system that “meets the oral health needs of all Americans and integrates oral health effectively into overall health.”
A core of public health and oral health advocates rallied to the call but the goals have remained elusive. Those who have worked for change know the inherent challenges of transforming the dental care system. They know that ultimately, meaningfully addressing oral health inequality will mean fundamental reform of the healthcare system that takes into account the long and separate history of American dentistry.
Since its beginnings as a profession in 1840, with the opening of the world’s first dental college in Baltimore, dentistry has evolved in isolation from the rest of the nation’s healthcare system.
Our heads may be attached to our bodies, but generations of dental and medical providers have been educated separately. They work in different worlds. And many patients get lost in between.
The fact that more than a million Americans a year turn to hospital emergency rooms for non-traumatic dental problems such as toothaches is a grim reminder of the disconnect between the dental and medical care systems. These visits cost roughly $1 billion a year, but the patients seldom get the services they need because ERs infrequently offer real dental care. Far too many fall through the cracks—or worse.
I started writing about oral health in 2007 as a reporter for the Washington Post, covering the story of Deamonte Driver, a twelve-year-old Maryland Medicaid beneficiary who died of complications from a dental abscess. The boy’s mother was seeking adequate care for his brother when Deamonte died. The children had been able to obtain immunizations and other routine health services but finding dental care was far more challenging in their poor community. Deamonte Driver’s highly publicized death spurred Congressional hearings and calls for more accountability and better performance by state Medicaid dental programs, leading to some reforms.
Yet grave deficiencies persist. Benefits, whether they are public or private, do not ensure access to care, particularly among low-income families coping with barriers including provider shortages, a lack of reliable transportation, and time off from work for appointments. Oral health literacy is not always a given, particularly in communities where basic care has been lacking sometimes for generations. Fatalism and fear of dental care are common. And even among those with dental coverage or middle-class incomes, skimpy benefits and high-out-of-pocket costs for care presents a major barrier to obtaining needed dental care.
Is there a better way?
Leading dental organizations including the ADA have contended that the causes of the United States’ silent epidemic lie not with the private practice system, but with the fact that Americans do not place a high enough value on oral health. Dental organizations representing the country’s more than 190,000 active dentists have supported increased spending on dental care, together with higher Medicaid reimbursement rates as ways of attracting more dentists to serve the poor. Yet the same dental groups have also long fought efforts to broaden access to care to underserved communities through the use of mid-level dental providers known as dental therapists. They contend that dental therapists lack the training to perform what are termed “irreversible surgical procedures” such as drilling and extracting teeth.
Advocates for dental therapists, however, compare these providers to nurse practitioners and say the workers, who deliver care as part of dentist-headed teams, could help bring timely and cost-effective preventive and restorative services to patients that the current private-practice system does not reach. In spite of opposition from dental organizations, dental therapists are now working in long-underserved tribal areas in Alaska, Washington State, and Oregon, as well as in poor and rural areas of the state of Minnesota. Grassroots groups and philanthropies are supporting their use in other states as well. But dental groups are pushing back hard. Battles are roiling statehouses across the country.
Dental organizations also have a long history of opposing efforts to nationalize the dental-care system. During the Great Depression, when leaders including President Franklin Delano Roosevelt were considering the establishment of a national health-insurance program, organized dentistry joined organized medicine in the fight against government-led healthcare.
“State dentistry is wrong in principle and would be disastrous in practice,” predicted the editors of the Journal of the American Dental Association in 1934, calling the idea “a monster of exploitation of the dental profession.”
The tensions between public efforts to expand healthcare and the interests of the private-practice system have endured. For instance, in the months leading up to the passage of President Barack Obama’s healthcare-reform law, the Affordable Care Act, the ADA urged members to let their lawmakers know that dentists would oppose any plan that “required health providers to participate,” that “directly or indirectly dictated fees for the private market,” or that “would lead to a government-run health system.”
Yet the ADA is not the only voice of dentists, and over the years, there have been dental leaders who have sought to reinvent the system. One was California dentist Max Schoen, who, in 1951, earned the distinction of being the first dentist to be called before the House Committee on Un-American Activities. Schoen would ultimately describe his life’s goal as “actively espousing health care for all regardless of the ability to pay.” Dental coverage did not exist until Schoen, working with the West Coast chapter of Harry Bridges’ International Longshore and Warehouse Union, invented a prepaid dental benefit program for the children of union members. Schoen set up a salaried, racially integrated group practice in the Los Angeles Harbor area to provide services to the children in return for fixed, capitated payments.
Schoen’s efforts were seen by some as a challenge. While he was working, a steady drumbeat of warnings issued from the pages of the Journal of the Southern California State Dental Journal. “Pale Pinks, Parlor Pinks on up through Crimsons . . . are threatening our livelihoods in the practice of dentistry,” noted a typical editorial.
But Schoen’s continuing innovations, geared toward bringing cost-effective care to workers, their families, and minority communities also attracted the interest of federal health authorities who were interested in finding ways to stretch healthcare dollars to meet wider needs. He went on to design plans to serve farmworkers, schools, and state governments. As he neared retirement, Schoen looked back on his career with hope. “I believe we proved anew . . . that it was perfectly possible and economically feasible to get almost all of any given population, regardless of socioeconomic status, to make regular use of preventive and therapeutic dental services.”
Schoen never gave up aspiring for a system of universal healthcare, and it is a dream that continues to drive oral health advocates today.
Nationally, children’s utilization of dental services under Medicaid has improved since Satcher’s Oral Health in America report in 2000 and since the death of Deamonte Driver in 2007. In 2016, dental leaders hailed as great progress the finding, reflected in federal data, that between 2000 and 2012, the percentage of Medicaid children receiving at least one dental service had climbed from 29 percent to 48 percent. But that still left more than half the children in the program—roughly 18 million—who received no care at all.
And while the Affordable Care Act succeeded in substantially reducing the rate of Americans without health benefits (albeit still leaving some 30 million uncovered, as of 2017), even with the Medicaid expansion and the inclusion of pediatric dental benefits as essential care for plans on insurance exchanges, the healthcare-reform law fell short in addressing oral health needs.
Recent research by the National Association of Dental Plans indicated that an estimated 74 million Americans (including nearly half of elderly and disabled Medicare beneficiaries) had no dental coverage in 2016—far higher than the rate of Americans who were medically uninsured.
And since the Republican sweep in the 2016 elections, many oral-health advocates worry that the fragile gains of recent years are at risk amid the ongoing conservative push to gut Obamacare and reduce spending on healthcare for the poor. Medicaid has been on “an unsustainable path,” White House Legislative Affairs Director Marc Short warned on NPR in late December. Cuts cannot be ruled out in order to make the program “sustainable for future generations.”
But at the very same time, progressive efforts to create a universal healthcare program are also growing.
Both single-payer plans now being considered by Congress include dental care. Vermont Senator Bernie Sanders, the lead sponsor of one of the bills, is no newcomer to the dental care debate. He has held hearings to examine oral health disparities and to explore the expansion of the dental workforce. He has called for reforms and sponsored legislation aimed at closing the dental divide.
“When we talk about the healthcare crisis in America,” Sanders has insisted, “we’ve got to also be talking about the dental crisis and how to address it.”
So the long struggle for oral health in America continues.
Mary Otto is an author and independent journalist based in Washington, D.C. She serves as oral health topic leader of the Association of Health Care Journalists. This essay is based, in part, on her book Teeth: The Story of Beauty, Inequality, and the Struggle for Oral Health in America (The New Press, 2017).